Abstract
Introduction All states in the US require hemoglobinopathy testing as part of the newborn screen (NBS) which incidentally identifies individuals with sickle cell trait (SCT). Each state has its own protocol for disclosure of SCT results to families (i.e., via primary care provider (PCP), public health nurse, direct mailing to family) with no standards for documentation in the electronic health record (EHR). Our past work showed that SCT is documented 53% of the expected rate within our EHR. Though gaps in documentation may not equate to lack of disclosure, such gaps demonstrate a risk for inadequate counseling and loss of data with transitions of care. Further, the majority of individuals with SCT are Black or Hispanic. Failure to disclose SCT may contribute to inequities in healthcare and hamper informed reproductive decision making.
Objective To identify barriers and facilitators to PCPs’ documentation and disclosure of SCT.
Methods A cross sectional survey of outpatient PCPs at 43 pediatric offices within a pediatric health system in Delaware, Pennsylvania, and Florida was conducted. Using Likert scales, rating scales, and free text response, the survey assessed PCP practices surrounding NBS results, attitudes toward SCT disclosure and documentation, and ranking of implementation strategies from the "Expert Recommendations for Implementing Change” project intended to increase SCT documentation and disclosure. Recruitment and survey administration was via REDCap. Lunch was provided to offices with >75% participation. Free text items were analyzed using qualitative methods. Descriptive statistics were used for other items. The study was approved by the IRB.
ResultsParticipants: Seventy-eight PCPs from 43 practices completed surveys (51% recruitment rate). Fourteen offices received lunch incentives. PCPs worked in their offices a mean of 7.1 years (SD 6.8y). Most (76%) identified as female and White (66%), with 17% Asian, 4% Black, and 12% Hispanic. Practice locations varied in percentages of patients insured by Medicaid (3-76%) or who identify as Black (2-91%).
NBS Results: Most PCPs had a process for reviewing NBS results with ~1/3 actively seeking results (i.e., log into a separate portal). The majority "always” checked a NBS during infancy but "never/occasionally” checked for an older new patient, before sports participation, or transition to adult medicine. All PCPs endorsed the importance for families and PCPs to know about hemoglobin traits but 14% thought a family may not want to know and 30% thought a family may have trouble understanding results. Nearly half (45%) thought a non-PCP should discuss results.
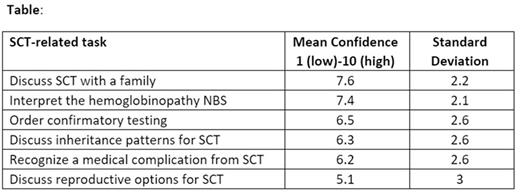
SCT: Almost all participants routinely discuss SCT during infancy. 16% routinely discuss it with adolescents and 56% "rarely/never” discuss SCT before transition to adult medicine. 10% "rarely/never” discuss inheritance patterns, but nearly one third "rarely/never” discuss possible medical complications and reproductive planning options. PCPs had varying confidence levels for several tasks (Table).
Barriers: In free text questions, PCPs identified barriers to discussing SCT (during infancy or adolescence) including PCP knowledge/comfort, adequate time, NBS availability, lack of "good” handouts, and family health literacy. Additional barriers included believing adolescents are not interested.
Potential Interventions: The highest ranked interventions to help increase the documentation and discussion of SCT included having a designated person to review the NBS, prompts within the EHR and templates for documentation, NBS program providing disclosure, longer appointment slots, educational sessions to increase PCP knowledge/comfort, and educational materials for families. Least helpful rated interventions included chart audits, incentives, leadership/society endorsements, or simulated discussions.
Conclusions Despite PCPs recognizing the importance of discussing SCT, they rarely do so outside of infancy and have varying degrees of confidence in doing so. PCPs recognized several system-based (i.e. time, EHR prompts) and personal barriers (i.e. confidence, knowledge) to discussing SCT. They expressed preferences for a range of potential implementation strategies. Real world studies are needed to determine whether strategies designed to address these barriers increase discussion and documentation of SCT across childhood and enhance care equity.
Disclosures
Smith-Whitley:Global Blood Therapeutics: Current Employment, Current equity holder in private company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal